Pharmacy Benefit Management (PBM) operations face mounting pressure from multiple directions. Drug costs have increased 5-7% annually over the past five years. Federal and state regulations change quarterly, requiring constant compliance monitoring. Meanwhile, prescription claim volumes continue growing as patient populations expand and formularies become more complex.
For many healthcare organizations, managing PBM operations entirely in-house has become unsustainable. Staff burnout increases. Error rates climb during peak periods. Compliance gaps emerge when internal teams can’t keep pace with regulatory changes.
BPO pharmacy benefit management offers a structured alternative—outsourcing specific PBM operational processes to specialized external partners who can handle scale, complexity, and compliance requirements more efficiently than stretched internal teams.
Key Points at a Glance
- What BPO means in PBM context: How outsourcing differs from traditional vendor relationships and why it’s a co-managed model, not a complete handoff
- Which functions are commonly outsourced: Claims processing, member support, compliance reporting, and data analytics—and why these specific areas benefit most from external expertise
- When outsourcing makes business sense: The volume thresholds, cost pressure points, and complexity triggers that indicate BPO is worth evaluating
- How to maintain control: Governance structures and SLAs that keep strategic decisions internal while operational execution scales externally
- Real implementation considerations: Timeline expectations, system integration requirements, and performance metrics that matter
What Is Pharmacy Benefit Management (PBM)?
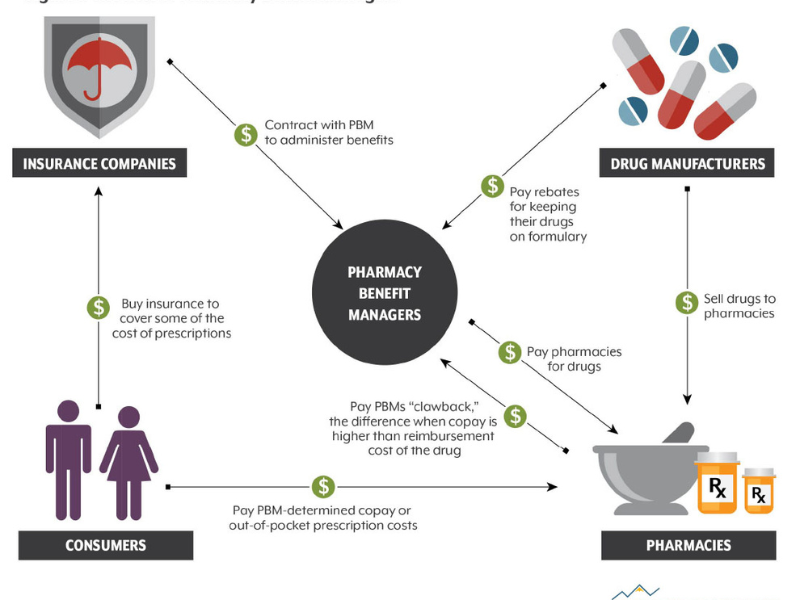
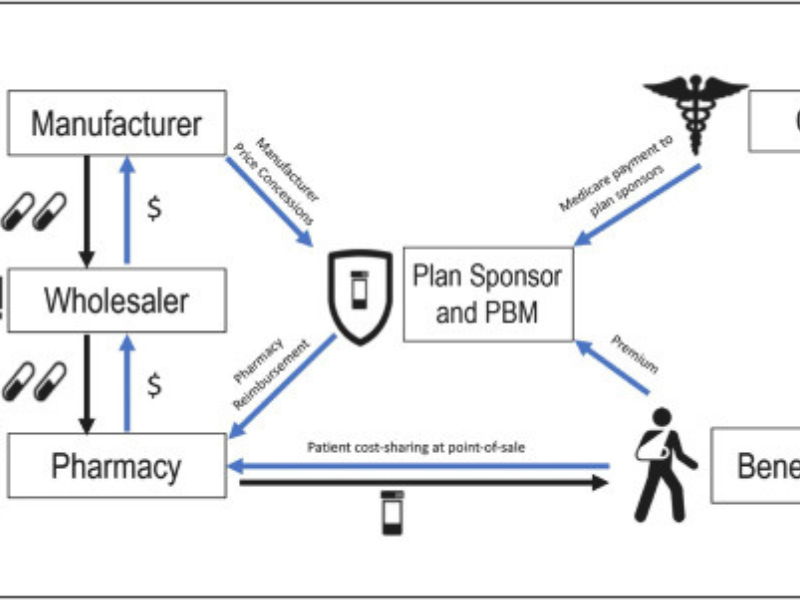
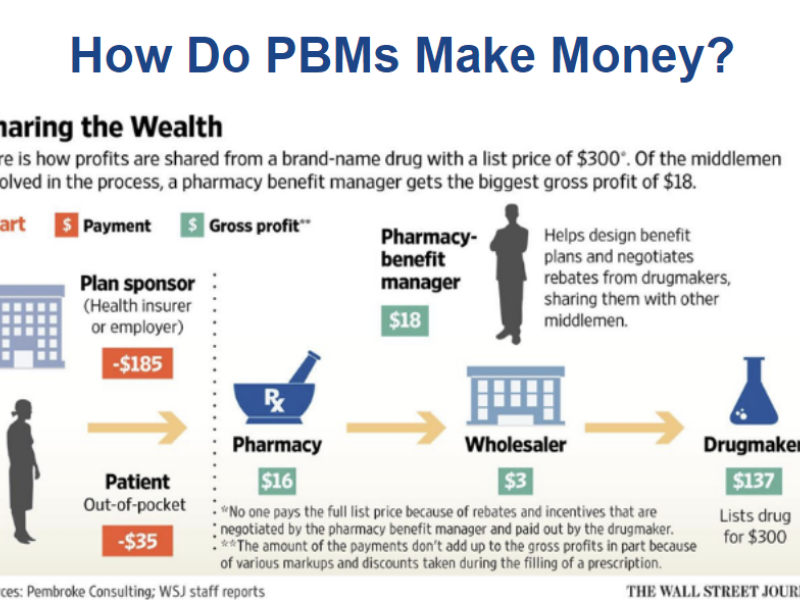
Pharmacy Benefit Management (PBM) sits between health plans, pharmacies, and patients—coordinating prescription drug benefits to control costs while ensuring patients can access needed medications.
Why PBM exists: Without PBM, health plans would negotiate directly with thousands of individual pharmacies and drug manufacturers—an impossible task at scale. PBM organizations centralize these negotiations, standardize processes, and manage the operational complexity of processing millions of prescription claims annually.
Core PBM responsibilities include:
Formulary management: Maintaining lists of covered medications, negotiating drug pricing with manufacturers, and establishing tier structures that balance cost with clinical effectiveness. When a new drug enters the market, PBM teams evaluate whether to add it to the formulary and at what cost-sharing level.
Claims processing: Validating coverage, checking eligibility, applying pricing rules, and adjudicating claims in real-time as patients fill prescriptions. A typical PBM processes 50,000-500,000+ claims daily depending on member population size.
Member and provider support: Answering benefit questions, resolving claim disputes, managing prior authorizations, and coordinating medication therapy management programs. Call volumes spike during annual enrollment periods and when formulary changes take effect.
Utilization monitoring: Tracking medication adherence, identifying potential drug interactions, flagging unusual prescribing patterns, and supporting population health initiatives.
What Is BPO in Pharmacy Benefit Management?
BPO (Business Process Outsourcing) in PBM means delegating specific operational functions—not strategic control—to external teams who specialize in executing these processes at scale.
What gets outsourced: High-volume, repeatable tasks like processing 100,000 prescription claims daily, answering 500+ member phone calls about benefit coverage, or generating monthly compliance reports across 15 different state regulations.
What stays internal: Strategic decisions about formulary design, benefit structure, vendor contract negotiations, and clinical policy development. Your organization retains full governance—BPO partners execute within parameters you define.
Example in practice: A regional health plan covers 500,000 members and processes 2 million prescription claims annually. Their internal PBM team of 8 people manages formulary strategy and vendor relationships. They partner with a BPO provider who handles:
- Daily claims processing (5,000-8,000 claims/day)
- Member support call center (200-400 calls/day)
- Compliance reporting (monthly state filings)
- Utilization analysis (weekly reports)
The internal team focuses on strategic initiatives—evaluating new drugs for formulary inclusion, negotiating manufacturer rebates, designing adherence programs. The BPO team executes the operational volume under defined SLAs.
In-House PBM vs BPO-Supported PBM
| Area | In-House Only | PBM with BPO Support |
|---|---|---|
| Staffing | Fixed headcount | Flexible capacity |
| Cost structure | High overhead | Variable, usage-based |
| 可扩展性 | 有限公司 | Built for growth |
| 合规监测 | Internal burden | Shared responsibility |
| Focus | Operational | Strategic |
Common Misconceptions
-
Reality: You retain complete governance authority. BPO partners operate under detailed SLAs that define performance standards, escalation protocols, and audit rights.
In practice: You approve all formulary changes. You set claims processing rules. You define member communication policies. The BPO team executes these decisions—they don’t make them. Monthly governance meetings review performance metrics, and you can adjust scope or terminate the relationship if standards aren’t met.
“Outsourcing creates compliance risks”
Reality: Certified BPO providers often strengthen compliance posture, not weaken it. They maintain dedicated compliance teams, undergo regular audits (SOC 2, HIPAA), and invest in systems that internal teams may lack budget for.
In practice: When HIPAA requirements changed in 2023, BPO providers updated systems and trained staff within weeks. Many in-house teams took 3-6 months to achieve full compliance due to competing priorities and resource constraints.
“BPO is a one-size-fits-all solution”
Reality: PBM outsourcing is modular and customizable. You choose which functions to outsource, define performance requirements, and adjust scope as needs change.
In practice: Some organizations outsource only claims processing. Others add member support but keep utilization management internal. A third group outsources everything except formulary strategy. The model adapts to your specific situation—there’s no mandatory “full outsourcing” requirement.
Co-Managed PBM Model
Most organizations use a co-managed model:
- Internal teams set strategy, policies, and oversight.
- BPO teams execute defined workflows under SLAs (service-level agreements).
例如
A regional payer keeps formulary strategy in-house while outsourcing claims processing and member support to a BPO partner.
How BPO Works Within PBM Operations
BPO integration into PBM follows a structured process designed to minimize disruption.
Step 1: Scope Definition
Most PBM outsourcing implementations follow a 12-16 week structured process designed to minimize disruption to ongoing operations.
Phase 1: Scope Definition & Planning (Weeks 1-3)
Your team and the BPO provider document exactly what will be outsourced and how success will be measured.
Typical scope decisions:
- Claims processing: All standard claims, or only retail (excluding specialty pharmacy)?
- Member support: Phone only, or also email and chat?
- Hours of operation: Business hours only (8am-6pm) or extended (7am-9pm)?
- 语言 English only, or also Spanish?
Performance standards defined:
- Claims turnaround: 98% processed within 24 hours
- Call answer rate: 90% of calls answered within 60 seconds
- First-contact resolution: 80% of member questions resolved without escalation
- Compliance: Zero HIPAA violations, monthly audit completion
Governance structure established:
- Weekly operational reviews (first 8 weeks)
- Monthly executive steering committee
- Quarterly business reviews with performance scorecards
- Escalation paths for urgent issues (defined response times)
Phase 2: System Integration (Weeks 4-8)
The BPO provider connects their systems to your existing PBM infrastructure—securely and with full data protection controls.
Technical integrations typically include:
Claims adjudication system: BPO staff need read/write access to process claims. Access is restricted by role—claims processors can’t view member financial data outside their assigned claims.
CRM/member portal: For viewing member history, benefit details, and claim status during support calls. BPO agents see only information necessary to resolve the specific inquiry.
Reporting and analytics platforms: To generate compliance reports, utilization summaries, and performance dashboards. Data exports are encrypted and access is logged for audit trails.
Security controls implemented:
- Multi-factor authentication for all BPO staff
- Role-based access (team leads see more data than individual processors)
- All activity logged with audit trails
- Automated alerts for unusual access patterns
- Annual penetration testing and security audits
Phase 3: Knowledge Transfer & Parallel Operation (Weeks 9-12)
Knowledge transfer (Weeks 9-10): Your internal team trains BPO staff on your specific processes, exceptions, and policies. This includes shadowing calls, reviewing sample claims, and documenting edge cases.
Parallel operation (Weeks 11-12): BPO team processes claims and handles calls while your internal team validates results. Example: BPO processes 500 claims daily, internal team audits random sample of 50 claims (10%) to verify accuracy before the BPO team takes over fully.
Typical parallel run results:
- Week 1 of parallel: 92-95% accuracy (learning curve)
- Week 2 of parallel: 97-99% accuracy (issues resolved)
- Week 3 checkpoint: If accuracy ≥98%, proceed to full transition
Phase 4: Full Transition & Ongoing Governance (Week 13+)
BPO team assumes full operational responsibility. Internal team shifts to oversight and strategic work.
Ramp-up schedule example:
- Week 13-14: 50% of volume through BPO, 50% internal (safety buffer)
- Week 15-16: 80% BPO, 20% internal
- Week 17+: 100% BPO for defined scope
Ongoing performance tracking:
Weekly dashboards monitor:
- Claims processed / errors caught / turnaround time
- Calls handled / average handle time / first-contact resolution rate
- Compliance audit results / security incidents (target: zero)
- Member satisfaction scores (post-call surveys)
Monthly governance meetings review trends and address issues before they impact service quality.
Step 2: System Integration
BPO teams connect securely to:
- Claims adjudication systems.
- CRM platforms (member interaction systems).
- Reporting and analytics tools.
Data access follows strict role-based controls.
Step 3: Process Transition
- Knowledge transfer from internal teams.
- Parallel run to validate accuracy.
- Gradual ramp-up to full volume.
Step 4: Ongoing Governance and KPIs
Performance is tracked through:
- Claim turnaround time.
- First-contact resolution rates.
- Compliance audit results.
- Member satisfaction scores.
Common PBM Functions Outsourced Through BPO Prescription Claims Processing

Claims processing is the highest-volume operational function in PBM—validating coverage, checking eligibility, applying pricing rules, and adjudicating claims in real-time as patients fill prescriptions at pharmacies.
Volume and complexity: A mid-size PBM processing claims for 500,000 members handles 5,000-8,000 claims daily. During peak periods (annual enrollment rollover, flu season, back-to-school), this can spike to 12,000-15,000 claims per day. Each claim must be processed within 2-5 seconds to avoid pharmacy delays.
Why this function is commonly outsourced:
Error reduction: Manual claims processing has a typical error rate of 2-4% (incorrect pricing, missed eligibility checks, wrong tier assignments). BPO teams using standardized workflows and automated validation reduce this to 0.3-0.8%—fewer claim rejections and member complaints.
Peak capacity handling: Staffing for peak volume means carrying excess capacity 8-9 months of the year. A BPO model scales capacity up during peak periods without permanent headcount increases. Example: During January enrollment rollover, BPO partner increases processing staff by 40% for 4-6 weeks, then scales back to baseline.
Faster turnaround: Industry standard for claims processing is 24-48 hours for standard claims, 72+ hours during peaks. BPO providers with dedicated teams consistently hit 98% of claims processed within 24 hours even during high-volume periods—maintaining service quality when internal teams would struggle.
Real impact: A health plan processing 2 million claims annually reduced operational costs by $380,000/year (25% savings) while improving claims accuracy from 96% to 99.2% after transitioning to BPO for claims processing.
Drug Formulary Management
BPO teams support formulary operations by:
- Maintaining updated drug lists.
- Coordinating changes with pharmacies and providers.
- Supporting utilization controls.
Strategic clinical decisions remain internal.
Medication Adherence Monitoring
Medication adherence (whether patients take drugs as prescribed) impacts outcomes and costs.
BPO supports adherence through:
- Outreach calls and reminders.
- Refill coordination.
- Member education programs.
Member and Provider Support Services
BPO-powered support centers handle:
| 频道 | Function |
|---|---|
| 电话 | Benefits explanation, claim status |
| 电子邮件 | Documentation and follow-ups |
| 聊天 | Quick eligibility questions |
| Portal | Self-service guidance |
Service quality is managed through SLAs and QA audits.
Data Analytics and Reporting
PBM generates large volumes of data.
BPO analytics teams:
- Convert raw data into performance reports.
- Track cost trends and utilization patterns.
- Support operational decision-making.
[Ảnh: Sample PBM performance dashboard]
Compliance and Regulatory Support
BPO providers support compliance with:
- HIPAA (patient data protection).
- SOC 2 (system and data controls).
- ISO/IEC 27001 (information security).
Key Benefits of BPO in Pharmacy Benefit Management

Cost Efficiency
Outsourcing reduces:
- Fixed staffing costs.
- Training and onboarding expenses.
- Technology maintenance overhead.
Costs scale with actual workload.
Operational Efficiency
Specialized BPO teams:
- Process higher volumes with fewer errors.
- Standardize workflows.
- Improve turnaround times.
This leads to smoother PBM operations.
Stronger Compliance Posture
Dedicated compliance teams:
- Monitor regulatory changes.
- Enforce consistent documentation.
- Support audit readiness.
This reduces organizational risk.
Scalability and Flexibility
BPO allows PBMs to:
- Scale up during enrollment peaks.
- Adjust capacity without restructuring.
- Support growth without operational strain.
Sharper Strategic Focus
With operational work outsourced, internal teams can focus on:
- Benefit design.
- Vendor negotiations.
- Member experience improvement.
When Does Outsourcing PBM Make Sense?

Outsourcing PBM is a strong option when:
- Claim volumes grow faster than staffing capacity.
- Compliance demands overwhelm internal teams.
- Cost pressure limits internal expansion.
- Member support volumes spike.
Partial vs Full Outsourcing
| 模型 | 最适合 |
|---|---|
| Partial | Targeted efficiency gains |
| Full | Rapid scale or turnaround |
When Not to Outsource
- Very small PBM operations.
- Highly customized, low-volume workflows.
- Organizations lacking governance maturity.
How to Choose the Right BPO Partner for PBM

Step-by-Step Evaluation
- Define clear PBM outsourcing goals.
- Verify healthcare-specific PBM experience.
- Assess compliance certifications.
- Review technology compatibility.
- Evaluate governance and reporting models.
Questions to Ask Vendors
- How do you handle PBM compliance audits?
- What KPIs do you guarantee?
- How do you manage data security?
Red Flags to Avoid
- Vague compliance claims.
- No PBM-specific case studies.
- Limited transparency in reporting.
Key Takeaways on BPO Pharmacy Benefit Management

- BPO pharmacy benefit management improves efficiency without sacrificing control.
- Outsourcing works best as a co-managed operational model.
- PBM BPO delivers cost savings, scalability, and compliance support.
- The right partner strengthens operations rather than replacing strategy.
FAQ: BPO Pharmacy Benefit Management

Is BPO pharmacy benefit management only for large organizations?
No. Mid-size payers and PBMs benefit most due to scalability needs.
Does outsourcing PBM increase compliance risk?
No. Certified BPO providers typically reduce compliance risk.
Can PBM outsourcing be partial?
Yes. Most organizations outsource only high-volume operational functions.
How long does PBM BPO implementation take?
Typically 8–16 weeks, depending on scope and systems.
结论
BPO pharmacy benefit management is no longer just a cost tactic.
It is a strategic operating model for modern PBM organizations.
If your PBM operations are stretched by growth, complexity, or regulation, it may be time to evaluate which processes belong in-house—and which perform better with a specialized BPO partner.
更多信息
- Call Center Resume Examples for 2026: ATS-Friendly Templates
- Customer Service Resume Examples: Guide with Metrics & ATS Tips
- 电子商务客户服务: Guide, Tools & 4-Week Action Plan